This systematic review aimed to explore the effects of upper cervical (C0/1, C1/2, or C2/3) mobilization/manipulation compared to sham or other inventions on pain, mouth opening and pressure pain thresholds in adults with temporomandibular joint (TMJ) dysfunction.
Four databases including Medline, CINAHL, EMBASE and The Cochrane Library were searched for randomised controlled trials (RCTs) published in English or translated using Google Translate into English. Eligible studies included people aged ≥ 18 years with TMJ pain of insidious onset and interventions utilising articular joint mobilizations and/or manipulations to the upper cervical spine compared to sham or other intervention. Outcome measures were pain on a visual analogue scale (VAS) or numeric pain rating scale (NPRS), maximal mouth opening (MMO) measured in millimetres using a range of motion (ROM) scale, and pressure pain threshold (PPT) of the temporalis and masseter muscles measured in kg/cm2 using a pressure algometer. Full text articles were independently screened by two reviewers with disagreements resolved through discussion. Minimal clinically important differences of a change of 2.0 points on the NPRS or VAS, 2.5mm for MMO, and 0.2kg/cm2 for the masticatory muscles. Authors were contacted to obtain insufficient or missing data. Risk of bias was independently evaluated by two reviewers using the Cochrane Risk of Bias Tool and resolved through discussion. Evidence quality and strength of recommendations for outcomes was assessed using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) system. A random-effects meta-analysis was conducted . Adverse events were not reported in the review.
Eight studies involving 437 participants were included. Four studies compared mobilization/manipulation with no intervention, three studies compared mobilization/manipulation with another intervention, and one study had multiple comparison groups. The average age of participants ranged from 20 to 47 years. Five trials included men and women, three included women only. The duration of TMJ symptoms was not stated in two trials, greater than one month in one trial, greater than three months in three trials, at least six months in one trial and between one and five years in one trial. Pain was measured in five trials, MMO in six trials, PPT of the masseter in four and of the temporalis in five trials. Treatment ranged from one to ten sessions and outcomes were assessed immediately after treatment to 32 weeks post-treatment. Of the included trials, one had low risk of bias, five has unclear risk of bias and two had high risk of bias.
Meta-analysis showed that mobilization/manipulation: reduced pain intensity compared to sham (MD = -1.93, 95% CI-3.61 to -0.24, n = 93, 2 trials, I2 = 83%) and compared to other interventions (MD = -1.03, 95% CI -1.73 to -0.33, n = 137, 3 trials, I2 = 27%); increased MMO compared to sham (MD = 2.11mm, 95% CI 0.26 to 3.96, n = 123, 3 trials, I2 = 0%) and compared to other interventions (MD = 2.25mm, 95% CI 1.01 to 3.48, n = 198, 4 trials, I2 = 0%). Mobilization/manipulation did not demonstrate a minimal clinically important difference for pain intensity nor MMO. Meta-analysis did not reveal an improvement in PPT for the masseter or temporalis muscles when comparing mobilization/manipulation to sham or other interventions. Using the GRADE approach, the certainty of evidence was moderate for pain and MMO, and low for PPT for the masticatory muscles.
Due to the low-moderate certainty evidence, a small number of trials, heterogeneity of included trials, and imprecise treatment estimates, it is unclear whether upper cervical spine mobilization/manipulation provides meaningful improvement in pain intensity, mouth opening, and pressure pain threshold in individuals with TMJ dysfunction.
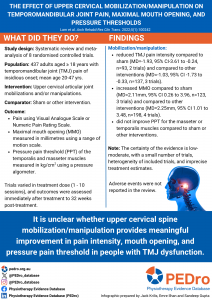
Lam AC, Liddle LJ, MacLellan CL. The effect of upper cervical mobilization/manipulation on temporomandibular joint pain, maximal mouth opening, and pressure pain thresholds: a systematic review and meta-analysis. Archives of Rehabilitation Research and Clinical Translation 2023 Nov;5(1):100242



